[ad_1]
Alfredo A. Sadun, MD, PhD, and colleagues conducted an international post-mortem study of human eyes treated with adeno-associated virus (AAV2)-based gene therapy for Leber hereditary optic neuropathy (LHON). The results were reported at the American Academy of Ophthalmology annual meeting in San Francisco.
The study takeaway, according to first author Dr Sadun, was that the results provided the first molecular and cellular evidence of successful gene transfection of retinal ganglion cells in humans. This effect, interestingly, was seen in both patient eyes despite the injection being only unilateral. Dr Sadun is from the Doheny Eye Institute, UCLA David Geffen School of Medicine, Los Angeles.
AAV2 gene therapy for LHON
LHON is a maternally inherited blinding mitochondrial genetic disease caused by the m.11778G>A mutation in the ND4 gene. The treatment with AAV2-based gene therapy compensates for the m.11778G>A mutation in affected retinal ganglion cells, the investigators explained.
Table. Patients treated with an intravitreal injection of lenadogene nolparvovec (AAV2-ND4) at 9×1010 vg in one eye and a sham injection in the fellow eye.
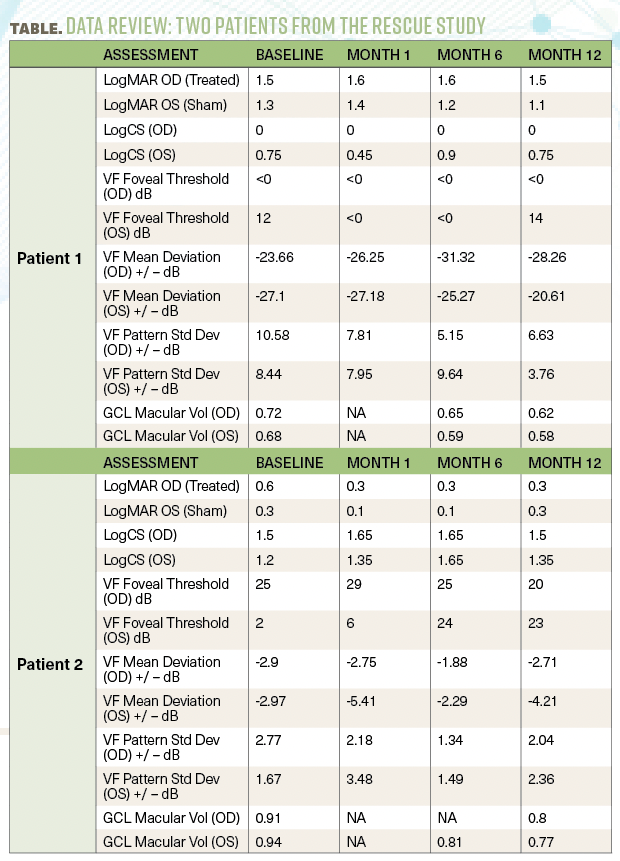
The study under discussion included 2 patients from the RESCUE clinical study. The patients were treated within 6 months following bilateral visual loss with an intravitreal injection of lenadogene nolparvovec (AAV2-ND4) at 9×1010 vg in one eye and a sham injection in the fellow eye [Table].
The investigators conducted post-mortem histopathologic and molecular analyses of the eyes using special immunohistochemistry, retinal laser microdissection and droplet digital polymerase chain reaction.
Study patients
Patient 1 was a 29-year-old man; patient 2 was a 22-year-old man. Both had LHON caused by the m.11778G>A ND4 mutation. Patient 1 died of acute alcohol toxicity. Patient 2 died of cardiac arrest.
In patient 1, the AAV2-ND4 transgene was distributed in both eyes but mostly in the right retina. In the non-injected eye, a minimal amount of transgene was found (1:200). Clinically, at 1 and 2 months after treatment, the right eye had moderate anterior chamber and vitreous intraocular inflammation; at 6 months and 1 year no intraocular inflammation was seen. The anterior chamber contained a few old pigmented keratitis precipitates and pigmented cells. At 6 months, the right eye had intermittent throbbing that resolved with sleep; at 1 year, both eyes burned constantly and were photosensitive.
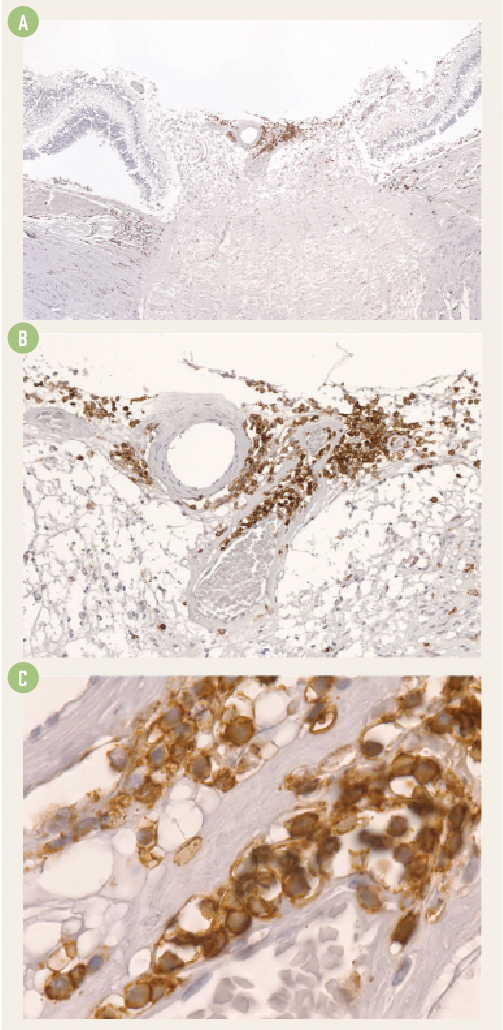
Histopathologically, focal areas of inflammation were seen in the temporal retina, presumably near the injection site, and, significantly, as an extensive angiocentric chronic lymphocytic infiltration at the optic nerve head. This correlated with the clinical intraocular infiltration.
Figure 1. Histopath slides showing the chronic angiocentric lymphocytic infiltration at low (A), medium (B) and high (C) magnification.
The investigators explained that the transgene in the inner half of the retina was about 100 times more concentrated than in the outer retina and was most abundant on the temporal retina near the macula. Transgene was not found in the retinal pigment epithelium, choroid, and optic nerve.
In contrast, in patient 2 no focal areas of inflammation were seen in the retina or optic nerve head in both eyes. At 2 months and 1 year after injection, the left eye had mild intermediate intraocular inflammation (no concomitant treatment).
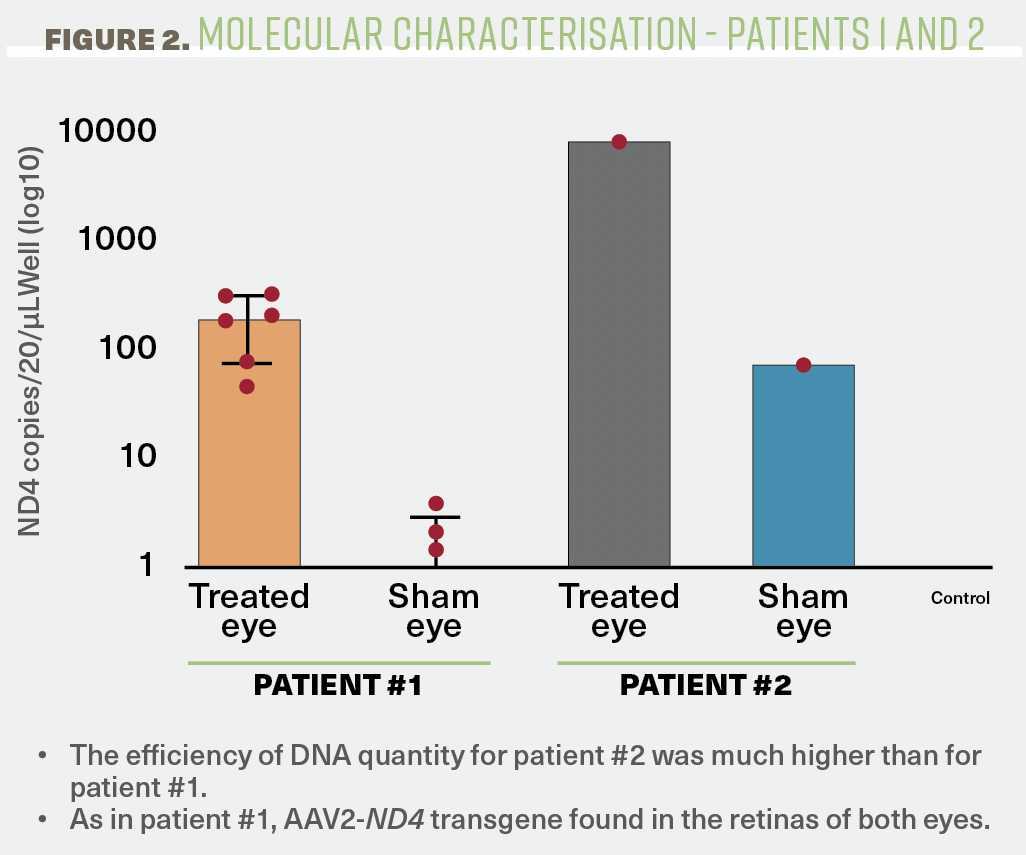
Commenting on the findings, the authors said, “The efficiency of DNA quantity for patient 2 was much higher than for patient 1. As in patient 1, AAV2-ND4 transgene was found in the retinas of both eyes.”
The key points gleaned from the 2 patients are as follows:
In patient 1, lymphocytic infiltration was observed in the temporal retina and especially around the blood vessels of the optic nerve head [Figures 1A, 1B and 1C]. AAV2-ND4 retinal transfection was evident in the injected eye and was detected at a much lower level in the contralateral eye.
In patient 2, in contrast, there was no histopathologic evidence of persistent inflammation. However, similar to patient 1, AAV2-ND4 transgene was found in the retinas of both eyes and at about the same ratio of 200 (injected eye) to 1 (fellow eye) [Figure 2].
Figure 2. AAV2-ND4 transgene distribution in both eyes.
(All images courtesy of Alfredo A. Sadun, MD, PhD)
“Taken together,” the investigators said, “this study provides the first evidence of successful gene transfection of retinal ganglion cells. It is intriguing that this occurred in both eyes after unilateral injection and further experiments at the optic chiasm and other parts of the brain of patient 2 are underway to determine the route of transfer.”
Reference
1. Alfredo A. Sadun, Nancy J. Newman, et al. Histopathological and molecular characterisations in ocular postmortem analyses following AAV2 gene therapy for LHON. Poster presented at: American Academy of Ophthalmology meeting; November 3-6, 2023; San Francisco, CA.
Alfredo A. Sadun, MD, PhD | e: alfredo.sadun@gmail.com
Alfredo A. Sadun, MD, PhD, holds the Flora L. Thornton Endowed Chair and is Chief at Doheny Eye Center-UCLA and Vice-Chair of Ophthalmology at UCLA. He is a recipient of the AAO Life Achievement Award and the ARVO Gold Fellow Award.
